Degenerative Joint Disease ICD 10 Code: A Complete Professional Guide
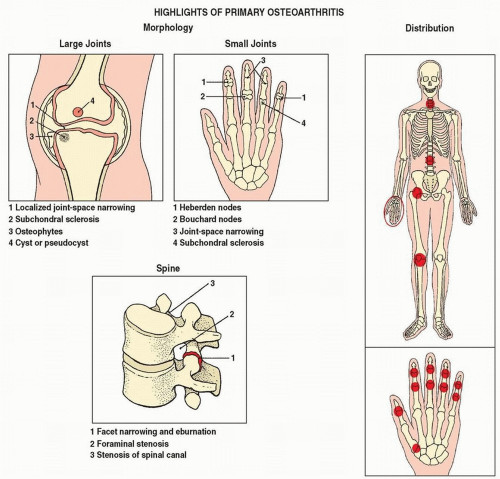
Degenerative joint disease icd 10 code, medically known as osteoarthritis (OA), is a chronic condition characterized by the progressive wear and tear of cartilage in the joints. It is the most common form of arthritis and one of the leading causes of disability worldwide, especially among older adults.
As the population ages and the demand for orthopedic and rheumatologic care increases, the need for accurate diagnosis and coding becomes more essential. The ICD-10-CM coding system, used in clinical documentation and medical billing, provides standardized codes to describe medical diagnoses such as DJD. This blog will cover what DJD is, how it is represented in ICD-10, and how healthcare professionals can use these codes effectively for documentation, billing, and patient care.
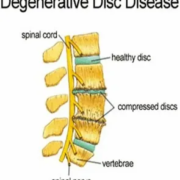
What Is Degenerative Joint Disease?
Degenerative joint disease icd 10 code is the gradual breakdown of articular cartilage, which acts as a cushion between bones in a joint. As the cartilage wears away, bones begin to rub together, leading to inflammation, pain, swelling, stiffness, and decreased range of motion. In advanced cases, bone spurs (osteophytes) may form, and joints can become severely deformed.
Commonly Affected Joints Include:
- Knees
- Hips
- Spine (cervical, thoracic, lumbar)
- Hands and fingers
- Feet and ankles
Typical Symptoms:
- Pain during or after activity
- Joint stiffness, especially in the morning
- Swelling or tenderness in the affected joint
- Cracking or grinding sensation (crepitus)
- Loss of flexibility and range of motion
Overview of ICD-10-CM
Degenerative joint disease icd 10 (International Classification of Diseases, 10th Revision, Clinical Modification) is the system used in the United States for coding diagnoses. Managed by the Centers for Medicare & Medicaid Services (CMS) and National Center for Health Statistics (NCHS), it is essential for:
- Clinical documentation
- Health insurance billing and claims
- Health statistics and research
- Disease tracking and surveillance
Each ICD-10 code is alphanumeric and represents a specific diagnosis or medical condition.
ICD-10-CM Codes for Degenerative Joint Disease
In the ICD-10-CM system, DJD is typically coded under the categories M15 to M19, which fall within the broader classification of arthrosis and osteoarthritis. Let’s explore the key codes in more detail.
Generalized or Polyarticular Osteoarthritis
| ICD-10 Code | Description |
|---|---|
| M15.0 | Primary generalized osteoarthritis |
| M15.4 | Secondary multiple osteoarthritis |
| M15.9 | Polyosteoarthritis, unspecified |
These codes are used when multiple joints are involved and there is no specific joint localization in the diagnosis.
Site-Specific DJD Codes
Osteoarthritis of the Knee
| ICD-10 Code | Description |
|---|---|
| M17.0 | Bilateral primary osteoarthritis of the knees |
| M17.10 | Unilateral primary osteoarthritis, unspecified knee |
| M17.11 | Unilateral primary osteoarthritis, right knee |
| M17.12 | Unilateral primary osteoarthritis, left knee |
Osteoarthritis of the Hip
| ICD-10 Code | Description |
|---|---|
| M16.0 | Bilateral primary osteoarthritis of the hips |
| M16.10 | Unilateral primary osteoarthritis, unspecified hip |
| M16.11 | Unilateral primary osteoarthritis, right hip |
| M16.12 | Unilateral primary osteoarthritis, left hip |
Hip osteoarthritis can severely impact mobility and often leads to hip replacement surgery in advanced cases.
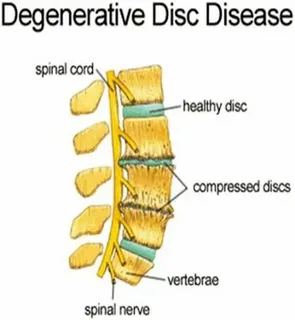
Spinal Osteoarthritis (Spondylosis)
| ICD-10 Code | Description |
|---|---|
| M47.812 | Spondylosis without myelopathy or radiculopathy, cervical region |
| M47.814 | Spondylosis without myelopathy or radiculopathy, thoracic region |
| M47.816 | Spondylosis without myelopathy or radiculopathy, lumbar region |
Spinal osteoarthritis may be accompanied by degenerative disc disease or spinal stenosis and can cause radiating pain into the arms or legs.
Hand and Wrist Osteoarthritis
| ICD-10 Code | Description |
|---|---|
| M18.0 | Primary osteoarthritis of the first carpometacarpal joint (thumb base) |
| M19.041 | Primary osteoarthritis, right hand |
| M19.042 | Primary osteoarthritis, left hand |
Hand osteoarthritis is especially common in postmenopausal women and may impact fine motor skills.
Foot and Ankle Osteoarthritis
| ICD-10 Code | Description |
|---|---|
| M19.071 | Primary osteoarthritis, right ankle and foot |
| M19.072 | Primary osteoarthritis, left ankle and foot |
Practical Coding Tips
Code to the Highest Specificity
Always include laterality (right, left, bilateral) when specified in the clinical documentation.
Differentiate Between Primary and Secondary DJD
- Primary DJD: develops without a known cause
- Secondary DJD: results from trauma, inflammation, or another disease
Combine with Symptom Codes (If Applicable)
For example:
- M25.561 – Pain in right knee
- M25.511 – Stiffness of right shoulder
Use symptom codes only when they are not integral to the diagnosis or need to be emphasized for care.
Example Case Studies
Case 1:
Patient: 62-year-old male with chronic bilateral knee pain.
Diagnosis: Bilateral primary knee osteoarthritis
Code: M17.0
Case 2:
Patient: 55-year-old female with DJD of the right hip following a fall 5 years ago.
Diagnosis: Post-traumatic osteoarthritis
Code: M16.11 (if primary) or M16.41 (if post-traumatic)
Case 3:
Patient: 70-year-old with back pain and radiological evidence of lumbar spondylosis.
Diagnosis: Lumbar spondylosis
Code: M47.816
Why ICD-10 Coding Matters
Accurate ICD-10 coding:
- Ensures proper reimbursement from insurance providers
- Helps track disease prevalence and trends
- Supports clinical research and public health initiatives
- Reduces medical errors and improves communication
Incorrect or non-specific coding can lead to:
- Claim denials
- Billing delays
- Incomplete medical records
- Legal risks
Conclusion
Degenerative joint disease icd 10 code is a major cause of pain and disability, but with precise ICD-10 coding, healthcare providers can document and treat it effectively. Whether it’s the knees, hips, spine, or hands, DJD must be coded with attention to detail—accounting for laterality, location, and severity.
For medical coders, clinicians, and healthcare administrators, mastering these codes is essential for efficient patient care, regulatory compliance, and optimized reimbursement.
Quick Reference: Common DJD ICD-10 Codes
| Joint Affected | Code Range | Examples |
|---|---|---|
| Generalized | M15.x | M15.0, M15.4 |
| Hip | M16.x | M16.0, M16.11 |
| Knee | M17.x | M17.0, M17.11 |
| Spine | M47.x | M47.812, M47.816 |
| Hand/Wrist | M18–M19.x | M18.0, M19.041 |
| Foot/Ankle | M19.07x | M19.071, M19.072 |