Degenerative Joint Disease ICD-10: A Complete Guide for Patients and Professionals
Degenerative joint disease icd 10, commonly known as osteoarthritis, is a widespread condition affecting millions globally. It involves the gradual breakdown of cartilage in joints, leading to pain, stiffness, and reduced mobility. For healthcare professionals, accurate diagnosis and documentation are essential—not only for treatment but also for billing, insurance, and research. That’s where the ICD-10 coding system plays a critical role.
In this blog, we will explore what degenerative joint disease is, how it’s classified in ICD-10, how coders and clinicians can correctly use these codes, and what patients should know about the implications of this coding.
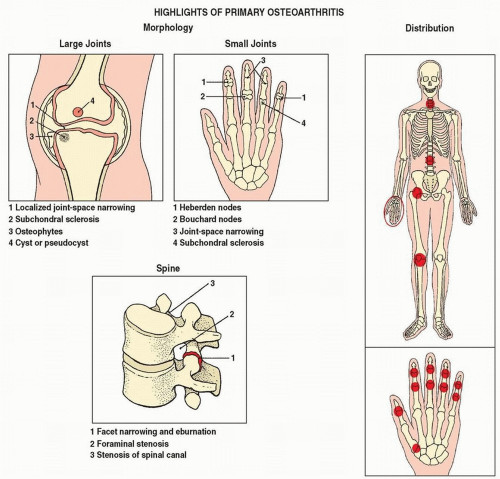
What is Degenerative Joint Disease?
Degenerative joint disease icd 10 code, or osteoarthritis, is the most common type of arthritis. It results from the wear and tear of joint cartilage and underlying bone, typically due to aging, overuse, trauma, or genetic predisposition.
Commonly Affected Joints:
- Knees
- Hips
- Spine (cervical, thoracic, lumbar)
- Hands and fingers
- Shoulders
Common Symptoms:
- Joint pain and tenderness
- Stiffness, especially in the morning
- Decreased range of motion
- Swelling in or around joints
- Crepitus (crackling or grinding noise)
Overview of ICD-10
ICD-10 stands for International Classification of Diseases, 10th Revision. It is maintained by the World Health Organization (WHO) and used globally for diagnosis coding.
In the United States, ICD-10-CM (Clinical Modification) is the version used for medical billing and coding. It helps to:
- Classify and track diseases
- Support public health statistics
- Ensure proper insurance reimbursement
- Streamline communication among healthcare providers
ICD-10 Codes for Degenerative Joint Disease
The primary ICD-10 code category for DJD is M15–M19, which falls under the “Arthrosis” codes.
Here’s a breakdown of the most relevant codes for different types and locations of degenerative joint disease:
Generalized Osteoarthritis
- M15.0 – Primary generalized (osteo)arthritis
- M15.4 – Secondary multiple arthritis
Osteoarthritis of Specific Joints
Knee:
- M17.0 – Bilateral primary osteoarthritis of knee
- M17.1 – Unilateral primary osteoarthritis of knee
- M17.5 – Other unilateral osteoarthritis of knee
Hip:
- M16.0 – Bilateral primary osteoarthritis of hip
- M16.1 – Unilateral primary osteoarthritis of hip
- M16.4 – Unilateral post-traumatic osteoarthritis of hip
Spine:
- M47.812 – Spondylosis without myelopathy or radiculopathy, cervical region
- M47.816 – Spondylosis without myelopathy or radiculopathy, lumbar region
Hand:
- M18.0 – Primary osteoarthritis of first carpometacarpal joint
- M19.041 – Primary osteoarthritis, right hand
- M19.042 – Primary osteoarthritis, left hand
Ankle & Foot:
- M19.071 – Primary osteoarthritis, right ankle and foot
- M19.072 – Primary osteoarthritis, left ankle and foot
Coding Tips and Guidelines
To ensure accurate documentation and reimbursement, follow these tips:
Use the Most Specific Code
Always code to the highest level of specificity, including laterality (right, left, bilateral) and joint location.
Identify the Type
Differentiate between:
- Primary osteoarthritis: no underlying cause
- Secondary osteoarthritis: due to trauma, other disease, or mechanical stress
Check for Associated Conditions
Some DJD cases involve:
- Spondylosis with radiculopathy (M47.2x)
- Osteoarthritis with effusion (fluid buildup)
- Post-traumatic changes (M16.1x, M17.1x)
Verify with Imaging
Radiographs (X-rays) or MRIs can support the diagnosis and help specify coding based on joint narrowing, bone spurs, or cartilage loss.
Example Scenarios
Example 1:
Patient: 68-year-old woman with chronic bilateral knee pain.
Diagnosis: Bilateral primary osteoarthritis of the knees.
ICD-10 Code: M17.0
Example 2:
Patient: 52-year-old man with unilateral post-traumatic osteoarthritis of the right hip.
ICD-10 Code: M16.11
Example 3:
Patient: 59-year-old female with osteoarthritis in cervical spine causing stiffness but no radiculopathy.
ICD-10 Code: M47.812
Causes and Risk Factors of DJD
Understanding the etiology helps in diagnosis and prevention.
Non-Modifiable Risk Factors:
- Age (over 50)
- Genetics/family history
- Female gender (especially after menopause)
Modifiable Risk Factors:
- Obesity
- Joint injuries (sports or occupational trauma)
- Repetitive stress (e.g., kneeling, lifting)
- Poor posture and spinal alignment
Treatment Options
Although there’s no cure, treatment can reduce symptoms and improve mobility:
Non-Surgical:
- NSAIDs (e.g., ibuprofen)
- Physical therapy
- Weight management
- Joint injections (steroids or hyaluronic acid)
- Bracing or orthotics
- Heat/cold therapy
Surgical:
- Joint replacement (hip or knee)
- Spinal decompression or fusion
- Arthroscopy (for specific joint repairs)
Patient Advice: Living with DJD
For patients diagnosed with DJD (especially noted on their medical records with ICD-10 codes), managing lifestyle is key:
- Stay active with low-impact exercises like swimming or walking
- Strengthen muscles around affected joints
- Use assistive devices (e.g., canes, orthotics) when needed
- Avoid repetitive joint strain
Early diagnosis with appropriate ICD-10 coding enables timely interventions and prevents further joint deterioration.
Final Thoughts
Degenerative joint disease icd 10 is a chronic, progressive condition that requires accurate medical documentation, especially for insurance claims, disability benefits, and treatment planning. The ICD-10 coding system plays a vital role in classifying the condition with precision.
Whether you’re a healthcare provider, medical coder, or patient, understanding the appropriate ICD-10 codes for DJD can streamline communication, improve care quality, and ensure correct billing and coverage.
Quick Reference: Common ICD-10 Codes for DJD
| Region | ICD-10 Code | Description |
|---|---|---|
| Knees | M17.0–M17.9 | Osteoarthritis of the knee |
| Hips | M16.0–M16.9 | Osteoarthritis of the hip |
| Spine | M47.81x | Spondylosis of spine (region-specific) |
| Hands | M18.0, M19.04x | Osteoarthritis of carpometacarpal joint, hand |
| Ankle/Foot | M19.07x | Osteoarthritis of ankle and foot |
| Generalized | M15.x | Primary/secondary generalized osteoarthritis |